ဒစဵုဒၞာဂဗ္ဘ
ဒစဵုဒၞာဂဗ္ဘ (Birth control) ဂှ် ဒှ်နဲကဲ ဟွံသေင်မ္ဂး မစကာအရပ်အရာမွဲမွဲ သွက်စဵုဒၞာ ညံင်ဟွံတန်ဂဗ္ဘ (ဝါ) ညံင်ဟွံတန်ပဋိသန္ဓိ (ဝါ) ညံင်ဟွံဂွံဗုင်ရ။[၁] ဒစဵုဒၞာဂဗ္ဘဂှ် ကောန်မၞိဟ်တအ် စကာကၠုင် နူကဵု အခိင်တမၠာတေအ်ရ၊ ဆဂး ဒစဵုဒၞာဂဗ္ဘ နကဵု နဲကဲမကၠောန်ကမၠောန်ခိုဟ်ဟ် ကေုာံ သက္ကုဘဲအန္တရာယ်ဂှ် စကလိဂွံ ပ္ဍဲကဵုခေတ် ၂၀ ဗွဝ်ကၠံရ။[၂] ပ္ဍဲကဵု အခိုက်ကၞာလ္ၚဵုဂှ်မ္ဂး ဒစဵုဒၞာဂဗ္ဘဂှ် ညးတအ်ဟွံဒုင်တဲ၊ ညးတအ် ညာတ်ကေတ် ဒှ်အရာမဗၠေတ်ကဵု ဒ္ဂေတ်ပြဝ၊ ဒစဵုဒစး ကုလညာတ်ဘာသာ ဟွံသေင်မ္ဂး လညာတ်ပရေင်ဍုင်ကွာန်ရ။
| ဒစဵုဒၞာဂဗ္ဘ | |
|---|---|
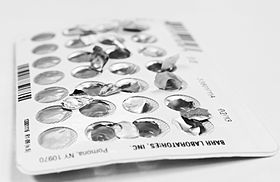 A package of birth control pills | |
| Other names | Contraception, fertility control |
| MeSH | D003267 |
ဒစဵုဒၞာဂဗ္ဘ နဲကဲ မကၠောန်ကမၠောန်ခိုဟ်အိုတ်ဂှ် ဒှ်နဲကဲ ဇမ္အး (sterilization) မဂွံအဓိပ္ပါယ် မဗပိုတ် ကတေင်ကောန် ပ္ဍဲကဵု မၞိဟ်တြုဟ်၊ ဟွံသေင်မ္ဂး ပ္ဍဲကဵု မၞိဟ်ဗြဴ မကော်ဂး intrauterine devices (IUDs)၊ ကေုာံ ဒစဵုဒၞာဂဗ္ဘ နမပတံစုတ် (implantable birth control) ရ။ ဒစဵုဒၞာဂဗ္ဘ နမပတံစုတ်ဂှ် ဒှ် နဲကဲ မဒုင်သဇိုင် ကုဓါတ်ဟောရ်မုန် (hormone-based methods) နွံနာနာသာ် မပတံကဵု ဂဥုဲစဵုဒၞာဲ (oral pills)၊ ပလာတ်သတာ (patches)၊ လကံက်ယောနိ (vaginal rings)၊ ကေုာံ ထပက်ဂဥုဲ (injections) ရ။ နကဵုနဲတၞဟ် မလေပ်ကၠောန်ကမၠောန် ဟွံခိုဟ်ကွေဟ်ဟ် နကဵု နဲမစဵုဒၞာ နကဵုကာယ မပတံကဵု နဲမစကာ ကောန်ဒေါမ် (condoms) မဓလိုက်စုတ် ပ္ဍဲအင်္ဂဇာတ် မၞိဟ်တြုဟ်၊ diaphragms ကဵု birth control sponges မဒှ်ဂရောပ် မစုတ်ပၠုပ် ပ္ဍဲယောနိမၞိဟ်ဗြဴ ကေုာံ နဲမစွံသတိ ကမၠောအ်မ (fertility awareness methods) မဒှ်နဲ မဝေင်ပါဲ ပ္ဍဲတ္ၚဲ ညးဗြဴဖျေဟ်ခၟာဲ။ နကဵုနဲ မကၠောန်ကမၠောန် အောန်အိုတ်ဂှ် ဒှ်နဲ ဂမ္စိုတ်သုက် (spermicides) မဒှ်ဂဥုဲ မစုတ်ပၠုပ် ပ္ဍဲယောနိမၞိဟ်ဗြဴ ကိုပ်ကၠာ ဟွံဆက်ဆောံလိင် အခိင်ညိည၊ မပကဵု ညံင်စၟသုက်ဂွံချိုတ် ကေုာံ နဲမၞိဟ်တြုဟ်ၜေတ်ပတိတ် ကိုပ်ကၠာ ဟွံစရိုဟ် (withdrawal by the male before ejaculation) ရ။ နကဵုနဲဇမ္အးဂှ် ဒှ်နဲ ကလေင်ကေတ်ဟွံဂွံတုဲ နဲတၞဟ်တအ်ဂှ် ဒှ်နဲကလေင်ဂွံ သီုဖအိုတ်တုဲ ဒှ်နဲ မပဒေါအ်ဇူလဝ် မွဲအခိင်ကာလရ။[၃] စကာ နဲ လိင်မသက်ကုဘဲ မပတံကဵု နဲမစကာကောန်ဒေါမ် မၞိဟ်တြုဟ် ကေုာံ ကောန်ဒေါမ်မၞိဟ်ဗြဴတအ်ဂှ် သီုဒှ် နဲမစဵုဒၞာ ညံင်ယဲဟွံဂွံကၠောအ် နကဵုမဆက်ဆောမ်လိင်ကီုရ။[၄] နဲဒစဵုဒၞာဂဗ္ဘတၞဟ်တအ်ဂှ် စဵုဒၞာကဵု ညံင်ယဲဟွံဂွံကၠောအ် နကဵုမဆက်ဆောမ်လိင် ဟွံမာန်ရ။[၅] ကြဴနူ ဆက်ဆောံလိင် သက်ကုစဵုဒၞာတုဲ အပ္ဍဲ အခိင်အကြာ ၇၂ ကဵု ၁၂၀ နာဍဳဂှ် စကာ နဲဒစဵုဒၞာဂဗ္ဘ ကာမံက်တိုန် (Emergency birth control) ဂွံမာန်ရ။[၆][၇] ညးလ္ၚဵုဂှ်ဟီု ဟွံမိက်ဂွံ ကောန်ဇာတ်မ္ဂး လ္ပဆက်ဆောံလိင် ရ။ ပညာလိင် မဒုင်သဇိုင် ကုပၞာဲမေထုန် ဟေင်ဂှ် ဒှ်အရာ မဂလိုင်ကဵု လၟိဟ် သၟာဲလေင် (သၟဝ်အာယုက် ၂၀) ဗုင်တိတ်/ သၟာဲလေင်တန်ဂဗ္ဘ မာန်ရ။ မေထုန်ဂှ် ဒှ်အရာသဘာဝ သတ်တအ်တုဲ ယဝ်ရ ညးသၟတ်တအ် ဟွံဂွံတီလဝ် နဲကဲဒစဵုဒၞာဂဗ္ဘမ္ဂး ယဝ်ရပညာလိင်ဂှ် ဒုင်သဇိုင် ကုနဲပၞာဲမေထုန်သၟး (ဝါ) ယဝ်ရ ဟီုလဝ် ဝေင်ပါဲဓဝ်မေထုန်သၟး ဆၜိုတ်ဏအ်ရမ္ဂး လၟိဟ်သၟာဲလေင်တန်ဂဗ္ဘဂှ် ဂၠိုင်တိုန်မာန်ရ။ ဟွံသေင်မ္ဂး ဟိုတ်နူ တန်အာဂဗ္ဘတုဲ ပ္ဍဲကဵု အာယုက်ဍောတ်တ်ဂှ် ဒးဒက်ဘဝအိန်ထံင်ဂှ် ဂၠိုင်ကၠုင်ရ။[၈][၉]
ပ္ဍဲဘဝသၟာဲလေင် (သၟဝ် အာယုက် ၂၀) ဂှ် ဒှ်ဟိုတ် မဖန်ဗဒှ်ကဵု ဘဝဒိုက်ဂတ်မာန်ရ။ နကဵုပညာလိင် ဗွဲမဍိုက်ပင် ကေုာံ မကလိဂွံ ဒစဵုဒၞာဂဗ္ဘဂှ် ဖန်ကဵု ညံင်ဂွံဖအောန်ဖျေဟ် ဒဒှ်မတန်ဂဗ္ဘ သက်ကုမနွံပၟိက် ပ္ဍဲကဵုဘဝသၟတ် မကော်ဂး ဘဝသၟာဲလေင်ဝွံမာန်ရ။[၁၀][၁၁]ပ္ဍဲကဵု ဘဝသၟတ်ဂှ် နဲကဲဒစဵုဒၞာဂဗ္ဘ မကလေင်ကေတ်ဂွံ မပတံကဵု စကာကောန်ဒေါမ်၊ စုတ်လကံက်ယောနိ၊ စုတ်တၞိင်ဟောရ်မုန်တအ်ဂှ် မလေပ်စကာ ဂွံဖအိုတ်တုဲ နကဵုနဲတအ်ဏအ် ဖအောန်ကဵု လၟိဟ်မတန်ဂဝ် ပ္ဍဲဘဝသၟာဲလေင်မာန်ရ။ နဲကဲမကလေင်ကေတ်ဟွံဂွံ (ဝါ) မကလေင်ကေတ်ဝါတ် ဗီုကဵု ဗပိုတ် ကတေင်ကောန်တအ်ဂှ် သွက်ညးသၟတ်တအ် ဟွံထေက်ကဵု စကာဏီရ။ ပါဲနူဂှ်တုဲ ကုညးဗြဴ မကလိဂွံကောန်ဇာတ်တၟိတၟိ ကောန်ဍောတ်ဒၟံင်ဏီ ဟွံမဲပၟိက် တန်ပဋိသန္ဓိဏီတအ်လေဝ် စကာ နဲဒစဵုဒၞာဂဗ္ဘတအ် ဂွံကီုရ။ မၞိဟ်ဗြဴတအ်ဂှ် ကြဴနူ သၠးဂၠံဂဝ်တုဲ အကြာ ပန်သတ္တဟ ကဵု တြဴသတ္တဟဂှ် တန်ဂၠံဂဝ်မာန်ဒၟံင်ရ။ ညးလ္ၚဵုထေင်ကေတ် ယဝ်ရ ဇကုဗမဴတှ်ကဵု ကောန်ၚာ်မ္ဂး တန်ဂၠံဂဝ်ဟွံမာန်ရ။ ဟိုတ်ဂှ်ရ သၠးဂၠံဂဝ်တုဲဗက်ဂှ် ယဝ်ရဇကုဟွံမဲပၟိက် တန်ဂၠံဂဝ်ဏီမ္ဂး ဒးစကာ နဲဒစဵုဒၞာဂဗ္ဘ နကဵုနဲလ္ၚဵုတအ်ဂှ် လဝါဲဂှ်ရ။ နဲလ္ၚဵုဂှ်မ္ဂး သၠးဂၠံဂဝ်တုဲ ဒးမင် မွဲလစုတ် ၜိုတ်တြဴဂိတုတုဲမ္ဂး စကာဂွံရ။[၁၂]
နဲကဲဂမၠိုင်
ပလေဝ်ဒါန်| Method | Typical use | Perfect use |
|---|---|---|
| No birth control | 85% | 85% |
| Combination pill | 9% | 0.3% |
| Progestin-only pill | 13% | 1.1% |
| Sterilization (female) | 0.5% | 0.5% |
| Sterilization (male) | 0.15% | 0.1% |
| Condom (female) | 21% | 5% |
| Condom (male) | 18% | 2% |
| Copper IUD | 0.8% | 0.6% |
| Hormonal IUD | 0.2% | 0.2% |
| Patch | 9% | 0.3% |
| Vaginal ring | 9% | 0.3% |
| MPA shot | 6% | 0.2% |
| Implant | 0.05% | 0.05% |
| Diaphragm and spermicide | 12% | 6% |
| Fertility awareness | 24% | 0.4–5% |
| Withdrawal | 22% | 4% |
| Lactational amenorrhea method (6 months failure rate) |
0–7.5%[၁၅] | <2%[၁၆] |
နဲကဲဒစဵုဒၞာဂဗ္ဘဂှ် နွံဒၟံင် သီုဖအိုတ် မသုန်နဲဂှ် နဲဒၞာခြာ (barrier methods)၊ နဲဂဥုဲဟောရ်မုန် (hormonal birth control)၊ နဲမဂြောပ်စုတ် (intrauterine devices) (IUDs)၊ နဲဇမ္အး (sterilization)၊ ကေုာံ နဲပၞာဲ (behavioral methods) တအ်ရ။ နဲလ္ၚဵုဂှ် စကာ ကိုပ်ကၠာ ဟွံသိပ်ဂၠိပ်မေထုန်၊ နဲလ္ၚဵုဂှ် စကာ အဃောမသိပ်ဂၠိပ်မေထုန်တုဲ နဲစဵုဒၞာကာတၟေင် (emergency contraceptive) ဂှ် ကြဴနူ သိပ်ဂၠိပ်မေထုန်တုဲ စဵုကဵုမသုန်တ္ၚဲ မြဴသာ်ဝွံ ဗီုမစကာ နဲကဲတအ်ဂှ် ဟွံတုပ် ရေင်သကအ်အိုတ်ရ။ နဲလ္ၚဵုဂှ် ဖန်လဝ် မွဲအလန်တုဲ ဍေဟ်ကၠောန်ကမၠောန် လလအ် ပွိုင်မွဲသၞာံ၊[၁၇] နဲလ္ၚဵု ဗီုကဵု နဲဗပိုတ် ကတေင်ကောန်တအ်ဂှ် ဍေဟ်ကၠောန်ကမၠောန် လလအ်ဇမၠိင်အာယုက်ရ။[၁၈]
နဲမကၠောန်ကမၠောန်ဂၠိုင်အိုတ် နဲဗပိုတ်သ္ၚိကောန်ဂှ် ဖန်လဝ် မွဲအလန်တုဲ ဟွံဒးအာ စဳစတ် ကုအစာဂဥုဲရ။[၁၉] နဲဂဥုဲဟောရ်မုန် မပတံကဵု ထပက်စုတ် ဂဥုဲ ပ္ဍဲကာယ၊ ပၠုပ်စုတ် ကိရိယာပ္ဍဲယောနိတအ်ဂှ် ဂွံပွိုင်မွဲသၞာံတုဲမ္ဂး ဒြဟတ်စဵုဒၞာ (ဝါ) ဒြဟတ်ကၠောန်ကမၠောန်ဍေဟ် အောန်စှ်ေအာ ၁% ရ။[၁၃] ပလာသတာ လကံက်ယောနိ၊ ကေုာံ နဲ lactational amenorrhea method (LAM) တအ်လေဝ် ပေင်မွဲသၞာံတုဲမ္ဂး ဒြဟတ်စဵုဒၞာ အောန်စှ်ေအာ ၁% ကီုရ။[၁၉]
နဲကဲဒစဵုဒၞာဂဗ္ဘတအ်ဂှ် နိသံသဍေဟ် ပကဵု အရာတၞဟ်တအ်မာန် နွံညိညကီုလေဝ် အန္တရာယ်ဟွံဇၞော် နူတန်ပဋိသန္ဓိ ပ္ဍဲဘဝသၟတ်ရ။[၁၉] ကြဴနူ မပဒေါအ် ဟွံသေင်မ္ဂး ပတိတ်ထောအ် ကိရိယာဒစဵုဒၞာဂဗ္ဘတအ်တုဲ အခေါင်မတန်ဂဗ္ဘမာန် အပ္ဍဲပွိုင်မွဲသၞာံဂှ် တုပ်သၟဟ်ကဵု မၞိဟ်ဟွံကေင် စကာလဝ် ကိရိယာတအ်ရ။ [၂၀]
ညးဗြဴလ္ၚဵု ဟိုတ်နူစကာ နဲကဲဒစဵုဒၞာဂဗ္ဘတုဲ ဗဒှ်ကဵု ပြသၞာ ပရေင်ထတ်ယုက်နွံကီုလေဝ် ကုညးပရေင်ထတ်ယုက်ခိုဟ်တအ်ဂှ် ဟိုတ်နူ ဒစဵုဒၞာဂဗ္ဘတုဲ ဗဒှ်ကဵု ပြသၞာပရေင်ထတ်ယုက်ဂှ် အောန်ကွေဟ်ရ။[၂၁] ပ္ဍဲသၞာံ ၂၀၀၉ ဂှ် နကဵု ဂကောံပရေင်ထတ်ယုက်ဂၠးကဝ် (WHO) ပ္တိတ်လဝ် နိသံသမကတဵုဒှ်မာန် ဇၟာပ်ပ် နဲကဲဒစဵုဒၞာဂဗ္ဘရ။ ဟိုတ်ဂှ်ရ ကိုပ်ကၠာ ဇကုဟွံရုဲစှ် နဲကဲလဵုမကိတ်ညဳကဵုဇကုဂှ် ချပ်ဂၞန် ကုသဝ်ဝန် စမ်ဆီတုဲ ရုဲစှ်မ္ဂး ခိုဟ်အိုတ်ရ။[၂၂]
ဂဥုဲဟောရ်မုန် (Hormonal)
ပလေဝ်ဒါန်နဲကဲ ဂဥုဲဟောရ်မုန်ဏအ်ဂှ် နွံဗီုပြင်နာနာသာ် မပတံကဵု ဂဥုဲသွုင် (oral pills) (လ္ၚဵုကော် ဂဥုဲကာဒ်)၊ တၞုင် ဒစဵုဒၞာဂဗ္ဘ (contraceptive implant) မထ္ပက်စုတ် ပ္ဍဲစၞာံ၊ ဂဥုဲတၞုင် (injectable contraceptives)၊ ပလာသတာ ဒစဵုဒၞာဂဗ္ဘ (contraceptive patch) မဗာန်လဝ် ပ္ဍဲဇကု၊ ပါ်ဟောရ်မုန် (hormonal IUD) မစုတ်ပၠုပ် ပ္ဍဲယောနိ ကေုာံ လကံက်ယောနိ (vaginal ring) လကံက်မပၠုပ်စုတ်လဝ် ပ္ဍဲယောနိမၞိဟ်ဗြဴရ။ [၂၃] ဂဥုဲသွုင်ဂှ် နွံၜါသာ်၊ မွဲဂှ် ညးကော်စ (combined oral contraceptive pill) မနွံကဵု ဓါတ်ၜါသာ် ဓါတ် estrogen ကဵု ဓါတ်progestin၊ မွဲဂကူပၠန်ဂှ် ဟိုတ်မနွံ ဆဓါတ်progestin သၟးတုဲ ညးကော်စ progestogen-only pill (လဆောဝ်ကော်စ ဂဥုဲကာဒ်ဍောတ် (minipills)။[၂၄]ဂဥုဲသီုၜါဂှ် အခိင်ကာလ မနွံကဵုဂဝ်ဂၞဴ (ဟိုတ်နူဟွံတီ) တုဲ သုင်ဒးမ္ဂး ဟွံကဵုအန္တရာယ် ကုကောန်ၚာ် သီုၜါရ။[၂၅]ဂဥုဲသီုၜါဂှ် ပကဵု ညံင်ခၟာဲ ပ္ဍဲမၞိဟ်ဗြဴ ဟွံဂွံအံင်ရ။[၂၆][၂၇]ဂဥုဲတအ်ဂှ် မလေပ်ပကဵု ဗီုကၠောန်ကမၠောန် ပ္ဍဲသ္ၚိကောန်တအ်ရ။[၂၇]ဂလိုင်ဍေဟ်မကၠောန်ကမၠောန်ဂှ် တန်တဴဒၟံင် ကုမၞိဟ်သွုင်ဂှ်ရ။ ဟိုတ်နူဒးသုင် အတိုင်စၞောန်တုဲ ယဝ်ရဝိုတ်စကီု၊ ယဝ်ရဟွံစှ်ေသၞောတ် အတိုင်စၞောန်မ္ဂး ဍေဟ်ဟွံကၠောန်ကမၠောန်ရ။[၂၅]
-
ဂဥုဲသွုင် သွက်စဵုဒၞာဂဗ္ဘ ပိ ရဲ မဗက်အာ အတိုင်လၟေင်တ္ၚဲကြက္ကဒိန် နူတ္ၚဲ စဆီကျာမကၠုင်။
-
ဂဥုဲသွုင် ဒစဵုဒၞာဂဗ္ဘ
-
ပလာသတာ ဒစဵုဒၞာဂဗ္ဘ
-
လကံက်ယောနိ NuvaRing
ဒၞာခြာ
ပလေဝ်ဒါန်နဲကဲဒၞာခြာဂှ် ဒှ်နဲကဲ မစကာ ကိရိယာ မဒၞာခြာ ညံင်စၟသုက် နူမၞိဟ်တြုဟ် ဟွံဂွံလုပ်စိုပ် ပ္ဍဲခၟာဲမၞိဟ်ဗြဴရ။[၂၈] နကဵုနဲဏအ်မ္ဂး စကာကောန်ဒေါမ်မၞိဟ်တြုဟ်ကီု သီုကဵု ကောန်ဒေါမ်မၞိဟ်ဗြဴ၊ cervical cap, Diaphragm, ကေုာံ ဂမ္စိုတ်သုက်တအ် ပါလုပ်ရ။[၂၈]
ပၞောဝ်ကဵု နဲဂမၠိုင်ဂှ် နဲစကာ ကောန်ဒေါမ်ဂှ် မၞိဟ်စကာဂၠိုင်အိုတ်ရ။[၂၉] ကောန်ဒေါမ်မၞိဟ်တြုဟ်ဂှ် ဓလိုတ်ပၠုပ် ပ္ဍဲအင်္ဂဇာတ်မၞိဟ်တြုဟ်တုဲ ဒၞာခြာထောအ် ညံင်ဍာ်သုက် နူမၞိဟ်တြုဟ် ဟွံဂွံကရိုဟ်လုပ်စိုပ်အာ ပ္ဍဲကဵု ယောနိမၞိဟ်ဗြဴပွံင်လိင် ကုမၞိဟ်တြုဟ်ဂှ်ရ။[၃၀] ကောန်ဒေါမ်ဂှ် ပ္ဍဲခေတ်တၟိဏအ် ဗွဲမဂၠိုင် ကၠောန်လဝ် နကဵုခၜိုတ် (latex) လ္ၚဵုဂှ် ကၠောန်လဝ် နကဵု (polyurethane)ရ။[၃၀] ကောန်ဒေါမ်မၞိဟ်ဗြဴလေဝ် ကၠောန်လဝ် နကဵုနာနာ မပ္တံကဵု ခၜိုတ်ကီုရ။[၃၁] ကောန်ဒေါမ်မၞိဟ်တြုဟ်ဂှ် ၚုဟ်မးတန်တုဲ စကာလောဲသွာ တုဲပၠန် သီုကဵု အန္တရာယ်အောန်ရ။[၃၂] ဖန်ဇန်လဝ် ညံင်ညးသၟတ်တအ် ဂွံကလိဂွံကောန်ဒေါမ်မာန်ဂှ် ဒှ်အရာ မဓလိုက်ကတဵုကဵု စိုတ်ရာဂလိင် ညးသၟတ်တအ် ညံင်ဂွံကတဵုဂၠိုင်ဟွံသေင်ရ။[၃၃]
ကောန်ဒေါမ်ဂှ် သီုစဵုဒၞာကဵု ညံင်ယဲမကၠောအ်ကၞာန် နကဵုမဆက်ဆောံလိင် မပ္တံကဵု ယဲအေအာင်ဒဳအေသ်တအ်ကီုရ။ ဆဂး ကောန်ဒေါမ် မကၠောန်လဝ် နကဵုကြုတ်တိရစ္ဆာန်တအ်ဂှ် စဵုဒၞာကဵု ယဲဟွံမာန်ရ။[၃][၃၄]
Contraceptive sponges combine a barrier with a spermicide.[၁၉] Like diaphragms, they are inserted vaginally before intercourse and must be placed over the cervix to be effective.[၁၉] Typical failure rates during the first year depend on whether or not a woman has previously given birth, being 24% in those who have and 12% in those who have not.[၁၃] The sponge can be inserted up to 24 hours before intercourse and must be left in place for at least six hours afterward.[၁၉] Allergic reactions[၃၅] and more severe adverse effects such as toxic shock syndrome have been reported.[၃၆]
-
ကောန်ဒေါမ် မၞိဟ်တြုဟ် သၟူလဝ်မွဲ။
-
ကောန်ဒေါမ်မၞိဟ်တြုဟ် မဟွံသၟူလဝ်မွဲ။
-
ကောန်ဒေါမ်မၞိဟ်ဗြဴ
-
A contraceptive sponge set inside its open package.
ကိရိယာမပၠုပ်ဂမၠိုင်
ပလေဝ်ဒါန်ကိရိယာ မပၠုပ်စုတ် မကော်ခဴစ ဗရိုတ်တဳ (ဟိုတ်မကၠောန်လဝ် နကဵုဗရိုတ် မနွံဗီုပြင် အက္ခရ်တဳ) ဂှ် ဒှ်ကိရိယာဍောတ်တ်မွဲ မပၠုပ်စုတ် စွံလဝ် ပ္ဍဲယောနိမၞိဟ်ဗြဴရ။ ကိရိယာဏအ်ဂှ် ဒှ်အရာ မကၠောန်ကမၠောန်ခို ပ္ဍဲအရာဒစဵုဒၞာဂဗ္ဘမွဲတုဲ ဂွံအခိင်လေဝ် လအ်ကီုရ။[၃၇] အရာဝွံ နွံၜါသာ် ဗရိုတ်အာင်ယူဒဳ (copper IUD) ကဵု levonorgestrel IUD။ ကိရိယာၜါဏအ်ဂှ် မွဲသၞာံမွဲအလန် ဒးကလေင်သၠာဲရ။ စကာပေင်အာ မွဲသၞာံတုဲမ္ဂး ဗရိုတ်အာင်ယူဒဳဂှ် ကၠောန်ကမၠောန်အောန်စှ်ေ ၜိုတ် ၀.၈% တုဲ levonorgestrel IUD ဂှ် အောန်စှ်ေ ၜိုတ် ၀.၂% ရ။[၃၈] ပၞောဝ်ကဵု ကိရိယာဒစဵုဒၞာဂဗ္ဘဂမၠိုင်မ္ဂး ကိရိယာဏအ်ဂှ် မၞိဟ်စကာဂၠိုင်တုဲ မၞိဟ်ဒးဂၞပ်လေဝ် ဂၠိုင်ကီုရ။[၃၉]အတိုင်စရင် ပ္ဍဲသၞာံ ၂၀၀၇ ဂှ်မ္ဂး မၞိဟ်မစကာကိရိယာဏအ် အလုံလိုက် နွံ ၁၈၀ မဳလဳယာန်ရ။[၄၀]
နကဵု ကိရိယာဝွံ ပ္ဍဲသၟာဲလေင်တအ်ကီုလေဝ် စကာဂွံ မသက်ကု ဘဲအန္တရာယ်၊[၃၉] တုဲပၠန် ဟိုတ်နူ စုတ်လဝ် ကိရိယာဏအ်တုဲ ကာလဇကုမိက်ဂွံဂွံကောန်ဇာတ်လေဝ် ဍေဟ်ဟွံ ဒှ်အခက်အခုဲရ။ and those who have and have not previously had children.[၄၁] တုဲပၠန် ဟိုတ်နူစုတ်လဝ် IUDs တုဲ ဍေဟ်ဟွံခ္ဍဳလျတ်ဒး ဍာ်တှ်တုဲ ကုညးမသၠးဂၠံဂဝ်တၟိ မနွံကဵု ကောန်တှ်တအ်လေဝ် ဟွံဒးမင် စုတ်ဂွံကီုရ။[၄၂]တုဲပၠန်် ကြဴနူ ကြဴနူပလီုဖျေဟ်ထောအ် ဂဝ်ဂၞဴတုဲ လွာဲဂှ် စုတ်ဂွံကီုရ။[၄၃][၄၄]ကာလမပတိတ်ထောအ်တုဲ ၜိုန်ရ စကာလဝ် အခိင်ဗွဲမလအ်ကီုလေဝ် ကလေင်ဒှ် အတိုင်ဓမ္မတာ (ဝါ) ကလိဂွံကောန်ဇာတ်မာန် လွာဲဂှ်ရ။[၄၅]
IUD ဗရိုတ်တအ်ဂှ် စုတ်တုဲ ဆီကျာကၠုင်ဂၠိုင် တုဲပၠန် ဂိဆီကျာ မလေပ် ဒှ်စမာန်ရ။ s may increase menstrual bleeding and result in more painful cramps,[၄၆]IUD ဟောရ်မုန်ဂှ် စုတ်တုဲမ္ဂး ဆီကျာကၠုင်အောန် ဟွံသေင်မ္ဂး ဆီကျာဒေါအ်အာ ဒှ်မာန်ရ။[၄၂]အရာမဂိတအ်ဂှ် သုင်ကေတ်ဂဥုဲဗၠးမာန်ရ။[၄၇] [၄၂][၄၇]နကဵု နဲပၠုပ်စုတ်ဝွံ စဵုဒၞာကဵု ယဲမကၠောအ်ကၞာန် နမဆက်ဆောံလိင် ဟွံမာန်ရ။[၄၈] IUDs appear to decrease the risk of ovarian cancer.[၄၉]
ဇမ္အး
ပလေဝ်ဒါန်ဇမ္အး ဟီုဂှ် ဒှ်အရာမဗပိုတ်ထောအ် ကတေင်ကောန် ပ္ဍဲကဵု ညးဗြဴကီု သီုကဵု မၞိဟ်တြုဟ်ရ။[၂] နဲဏအ်ဂှ် ဒှ်နဲမစိုပ်တရဴဂၠိုင်အိုတ်တုဲ ယဝ်ရ ဗပိုတ်ကတေင်ကောန် မၞိဟ်ဗြဴမ္ဂး သီုဖအောန်ကဵု ညံင်ဟွံဂွံဒှ် ကေန်သာသ္ၚိကောန် မာန်ကီုရ။[၂] ကြဴနူ ဗပိုတ်ကတေင်တုဲ ၜိုတ်မွဲသတ္တဟ ဟွံသေင်မ္ဂး ၜါသတ္တဟဂှ် ဗုင်မလေပ်ခအံင်ဒှ်မာန်ရ။[၅၀] နကဵုနဲဏအ်ဂှ် စဵုဒၞာကဵု ယဲမကၠောအ်ကၞာန် နူကဵု မဆက်ဆောံလိင် ဟွံမာန်ကီုရ။[၂]
နကဵုနဲဏအ်ဂှ် ဟိုတ်နူမကလေင်ကေတ် ဟွံလောဲဂှ်ရ မၞိဟ်တြုဟ်တအ် ကၠောန်စအောန်တုဲ ဗွဲမဂၠိုင် မၞိဟ်ဗြဴလတူအာယုက် ၃၀ ကလိဂွံကောန်ဇာတ်တုဲတအ် မလေပ်ကၠောန်စဂၠိုင်ရ။[၂]
နကဵုနဲဏအ်ဂှ် ၜိုန်ရ ဟီုလဝ် ဒှ်နဲမဗပိုတ်ထာဝရကီုလေဝ် ကလေင်ဆက်ဂွံမာန်ဒၟံင်ဏီရ။ ကြဴနူ မကလေင်ဆက်တုဲ အခေါင်မကလိဂွံ ဂဝ်ဂၞဴပၠန် နွံဒၟံင် အကြာ ၃၁ ကဵု ၈၈ က္ဍိုပ်ကၠံရ။[၅၁]
Behavioral
ပလေဝ်ဒါန်Behavioral methods involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present.[၅၂] If used perfectly the first-year failure rate may be around 3.4%, however if used poorly first-year failure rates may approach 85%.[၅၃]
Fertility awareness
ပလေဝ်ဒါန်Fertility awareness methods involve determining the most fertile days of the menstrual cycle and avoiding unprotected intercourse.[၅၂] Techniques for determining fertility include monitoring basal body temperature, cervical secretions, or the day of the cycle.[၅၂] They have typical first-year failure rates of 24%; perfect use first-year failure rates depend on which method is used and range from 0.4% to 5%.[၁၃] The evidence on which these estimates are based, however, is poor as the majority of people in trials stop their use early.[၅၂] Globally, they are used by about 3.6% of couples.[၅၄] If based on both basal body temperature and another primary sign, the method is referred to as symptothermal. First-year failure rates of 20% overall and 0.4% for perfect use have been reported in clinical studies of the symptothermal method.[၅၅][၁၃] A number of fertility tracking apps are available, as of 2016, but they are more commonly designed to assist those trying to get pregnant rather than prevent pregnancy.[၅၆]
Withdrawal
ပလေဝ်ဒါန်The withdrawal method (also known as coitus interruptus) is the practice of ending intercourse ("pulling out") before ejaculation.[၅၇] The main risk of the withdrawal method is that the man may not perform the maneuver correctly or in a timely manner.[၅၇] First-year failure rates vary from 4% with perfect usage to 22% with typical usage.[၁၃] It is not considered birth control by some medical professionals.[၁၉]
There is little data regarding the sperm content of pre-ejaculatory fluid.[၅၈] While some tentative research did not find sperm,[၅၈] one trial found sperm present in 10 out of 27 volunteers.[၅၉] The withdrawal method is used as birth control by about 3% of couples.[၅၄]
Abstinence
ပလေဝ်ဒါန်Sexual abstinence may be used as a form of birth control, meaning either not engaging in any type of sexual activity, or specifically not engaging in vaginal intercourse, while engaging in other forms of non-vaginal sex.[၆၀][၆၁] Complete sexual abstinence is 100% effective in preventing pregnancy.[၆၂][၆၃] However, among those who take a pledge to abstain from premarital sex, as many as 88% who engage in sex, do so prior to marriage.[၆၄] The choice to abstain from sex cannot protect against pregnancy as a result of rape, and public health efforts emphasizing abstinence to reduce unwanted pregnancy may have limited effectiveness, especially in developing countries and among disadvantaged groups.[၆၅][၆၆]
Deliberate non-penetrative sex without vaginal sex or deliberate oral sex without vaginal sex are also sometimes considered birth control.[၆၀] While this generally avoids pregnancy, pregnancy can still occur with intercrural sex and other forms of penis-near-vagina sex (genital rubbing, and the penis exiting from anal intercourse) where sperm can be deposited near the entrance to the vagina and can travel along the vagina's lubricating fluids.[၆၇][၆၈]
Abstinence-only sex education does not reduce teenage pregnancy.[၅][၆၉] Teen pregnancy rates and STI rates are generally the same or higher in states where students are given abstinence-only education, as compared with comprehensive sex education.[၆၉] Some authorities recommend that those using abstinence as a primary method have backup methods available (such as condoms or emergency contraceptive pills).[၇၀]
Lactation
ပလေဝ်ဒါန်The lactational amenorrhea method involves the use of a woman's natural postpartum infertility which occurs after delivery and may be extended by breastfeeding.[၇၁] This usually requires the presence of no periods, exclusively breastfeeding the infant, and a child younger than six months.[၁၆] The World Health Organization states that if breastfeeding is the infant's only source of nutrition, the failure rate is 2% in the six months following delivery.[၇၂] Six uncontrolled studies of lactational amenorrhea method users found failure rates at 6 months postpartum between 0% and 7.5%.[၇၃]ထာမ်ပလိက်:Update inline Failure rates increase to 4–7% at one year and 13% at two years.[၇၄] Feeding formula, pumping instead of nursing, the use of a pacifier, and feeding solids all increase its failure rate.[၇၅] In those who are exclusively breastfeeding, about 10% begin having periods before three months and 20% before six months.[၇၄] In those who are not breastfeeding, fertility may return four weeks after delivery.[၇၄]
Emergency
ပလေဝ်ဒါန်Emergency contraceptive methods are medications (sometimes misleadingly referred to as "morning-after pills")[၇၆] or devices used after unprotected sexual intercourse with the hope of preventing pregnancy. Emergency contraceptives are often given to victims of Rape[၆] They work primarily by preventing ovulation or fertilization.[၂][၇၇] They are unlikely to affect implantation, but this has not been completely excluded.[၇၇] A number of options exist, including high dose birth control pills, levonorgestrel, mifepristone, ulipristal and IUDs.[၇၈] Providing emergency contraceptive pills to women in advance does not affect rates of sexually transmitted infections, condom use, pregnancy rates, or sexual risk-taking behavior.[၇၉][၈၀] All methods have minimal side effects.[၇၈]
Levonorgestrel pills, when used within 3 days, decrease the chance of pregnancy after a single episode of unprotected sex or condom failure by 70% (resulting in a pregnancy rate of 2.2%).[၆] Ulipristal, when used within 5 days, decreases the chance of pregnancy by about 85% (pregnancy rate 1.4%) and is more effective than levonorgestrel.[၆][၇၈][၈၁] Mifepristone is also more effective than levonorgestrel, while copper IUDs are the most effective method.[၇၈] IUDs can be inserted up to five days after intercourse and prevent about 99% of pregnancies after an episode of unprotected sex (pregnancy rate of 0.1 to 0.2%).[၂][၈၂] This makes them the most effective form of emergency contraceptive.[၈၃] In those who are overweight or obese, levonorgestrel is less effective and an IUD or ulipristal is recommended.[၈၄]
Dual protection
ပလေဝ်ဒါန်Dual protection is the use of methods that prevent both sexually transmitted infections and pregnancy.[၈၅] This can be with condoms either alone or along with another birth control method or by the avoidance of penetrative sex.[၈၆][၈၇]
If pregnancy is a high concern, using two methods at the same time is reasonable.[၈၆] For example, two forms of birth control are recommended in those taking the anti-acne drug isotretinoin or anti-epileptic drugs like carbamazepine, due to the high risk of birth defects if taken during pregnancy.[၈၈][၈၉]
References
ပလေဝ်ဒါန်- ↑ Definition of Birth control. MedicineNet. Archived from the original on August 6, 2012။ Retrieved on August 9, 2012။
- ↑ ၂.၀ ၂.၁ ၂.၂ ၂.၃ ၂.၄ ၂.၅ ၂.၆ The Johns Hopkins manual of gynecology and obstetrics။
- ↑ ၃.၀ ၃.၁ World Health Organization Department of Reproductive Health and Research (2011). Family planning: A global handbook for providers: Evidence-based guidance developed through worldwide collaboration, Rev. and Updated, Geneva: WHO and Center for Communication Programs. ISBN 978-0-9788563-7-3။
- ↑ Taliaferro (2011). "We have the evidence to enhance adolescent sexual and reproductive health—do we have the will?".
- ↑ ၅.၀ ၅.၁ Chin (2012). "The Effectiveness of Group-Based Comprehensive Risk-Reduction and Abstinence Education Interventions to Prevent or Reduce the Risk of Adolescent Pregnancy, Human Immunodeficiency Virus, and Sexually Transmitted Infections".
- ↑ ၆.၀ ၆.၁ ၆.၂ ၆.၃ Gizzo. "Nowadays which emergency contraception? Comparison between past and present: latest news in terms of clinical efficacy, side effects and contraindications".
- ↑ Selected practice recommendations for contraceptive use, 2nd, Geneva: World Health Organization. ISBN 978-92-4-156284-3။
- ↑ "Interventions to reduce unintended pregnancies among adolescents: systematic review of randomised controlled trials" .
- ↑ Duffy (2008). "Government Support for Abstinence-Only-Until-Marriage Education".
- ↑ Black (2012). "Pregnancy in adolescents": xi, 123–38.
- ↑ Rowan (2012). "Contraception for primary care providers": x–xi, 95–110.
- ↑ World Health Organization Department of Reproductive Health and Research (2011). Family planning: A global handbook for providers: Evidence-based guidance developed through worldwide collaboration, Rev. and Updated, Geneva: WHO and Center for Communication Programs, 260–300. ISBN 978-0-9788563-7-3။
- ↑ ၁၃.၀ ၁၃.၁ ၁၃.၂ ၁၃.၃ ၁၃.၄ ၁၃.၅ Trussell, James (May 2011). "Contraceptive failure in the United States". Contraception 83 (5): 397–404. doi:. PMID 21477680.
Trussell, James (2011). "Contraceptive efficacy", Contraceptive technology, 20th revised, New York: Ardent Media, 779–863. ISBN 978-1-59708-004-0. OCLC 781956734။ - ↑ "U.S. Selected practice recommendations for contraceptive use, 2013: adapted from the World Health Organization Selected practice recommendations for contraceptive use, 2nd edition" (June 21, 2013). MMWR Recommendations and Reports 62 (5): 1–60. PMID 23784109.
- ↑ "Lactational amenorrhoea method for family planning" (12 October 2015). The Cochrane Database of Systematic Reviews (10): CD001329. doi:. PMID 26457821.
- ↑ ၁၆.၀ ၁၆.၁ Blenning, CE (Dec 15, 2005). "An approach to the postpartum office visit". American Family Physician 72 (12): 2491–96. PMID 16370405.
- ↑ Gordon Edlin (2000). Essentials for health and wellness, 2nd, Sudbury, MA: Jones and Bartlett, 161. ISBN 978-0-7637-0909-9။
- ↑ (2012) Dewhurst's textbook of obstetrics & gynaecology, 8th, Chichester, West Sussex: Wiley-Blackwell, 508. ISBN 978-0-470-65457-6။
- ↑ ၁၉.၀ ၁၉.၁ ၁၉.၂ ၁၉.၃ ၁၉.၄ ၁၉.၅ ၁၉.၆ (2012) "Contraception and sterilization", Williams gynecology, 2nd, New York: McGraw-Hill Medical, 132–69. ISBN 978-0-07-171672-7။
- ↑ Mansour, D (November 2011). "Fertility after discontinuation of contraception: a comprehensive review of the literature". Contraception 84 (5): 465–77. doi:. PMID 22018120.
- ↑ Department of Reproductive Health and Research, Family and Community (2004). Selected practice recommendations for contraceptive use., 2nd, Geneva: World Health Organization, Chapter 31. ISBN 978-92-4-156284-3။ Archived ဂျူလာင် ၁၈, ၂၀၁၃ at the Wayback Machine
- ↑ Organization, World Health (2009). Medical eligibility criteria for contraceptive use, 4th, Geneva: Reproductive Health and Research, World Health Organization, 1–10. ISBN 978-92-4-156388-8။ Archived ဂျူလာင် ၉, ၂၀၁၂ at the Wayback Machine
- ↑ Mackenzie၊ James။ "The male pill? Bring it on"၊ December 6, 2013။ May 20, 2014 တင်နိဿဲဏအ် စၟဳစၟတ်တုဲ။ Archived from the original on May 21, 2014။
- ↑ Ammer, Christine (2009). "oral contraceptive", The encyclopedia of women's health, 6th, New York: Facts On File, 312–15. ISBN 978-0-8160-7407-5။
- ↑ ၂၅.၀ ၂၅.၁ နိဿဲ ဗၠေတ် - Invalid
<ref>tag; no text was provided for refs namedWHO_FP2011p10 - ↑ (2011) "Combined oral contraceptives (COCs)", Contraceptive technology, 20th revised, New York: Ardent Media, 249–341 [257–58]. ISBN 978-1-59708-004-0. OCLC 781956734။
- ↑ ၂၇.၀ ၂၇.၁ (2011) "5 Second-Tier Contraceptive Methods—Very Effective", Williams gynecology, 2nd, New York: McGraw-Hill Medical. ISBN 978-0-07-171672-7။
- ↑ ၂၈.၀ ၂၈.၁ Neinstein, Lawrence (2008). Adolescent health care : a practical guide, 5th, Philadelphia: Lippincott Williams & Wilkins, 624. ISBN 978-0-7817-9256-1။
- ↑ Chaudhuri (2007). Practice Of Fertility Control: A Comprehensive Manual, 7th, Elsevier India, 88. ISBN 978-81-312-1150-2။
- ↑ ၃၀.၀ ၃၀.၁ Hamilton, Richard (2012). Pharmacology for nursing care, 8th, St. Louis, MO: Elsevier/Saunders, 799. ISBN 978-1-4377-3582-6။
- ↑ (2010) Facts for life, 4th, New York: United Nations Children's Fund, 141. ISBN 978-92-806-4466-1။
- ↑ Pray, Walter Steven (2005). Nonprescription product therapeutics, 2nd, Philadelphia: Lippincott Williams & Wilkins, 414. ISBN 978-0-7817-3498-1။
- ↑ "Condom Use by Adolescents" (October 28, 2013). Pediatrics 132 (5): 973–81. doi:. PMID 28448257.
- ↑ Preventing Sexually Transmitted Infections (STIs) (February 2017). Archived from the original on 27 July 2020။ Retrieved on 22 June 2020။
- ↑ Kuyoh, MA (January 2003). "Sponge versus diaphragm for contraception: a Cochrane review.". Contraception 67 (1): 15–18. doi:. PMID 12521652.
- ↑ Organization, World Health (2009). Medical eligibility criteria for contraceptive use, 4th, Geneva: Reproductive Health and Research, World Health Organization, 88. ISBN 978-92-4-156388-8။
- ↑ "Effectiveness of Long-Acting Reversible Contraception" (2012). New England Journal of Medicine 366 (21): 1998–2007. doi:. PMID 22621627.
- ↑ (March 28, 2012) The Johns Hopkins manual of gynecology and obstetrics, Department of Gynecology and Obstetrics, The Johns Hopkins University School of Medicine, Baltimore Maryland, 4th, Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 232. ISBN 978-1-60547-433-5။
- ↑ ၃၉.၀ ၃၉.၁ Committee on Adolescent Health Care Long-Acting Reversible Contraception Working Group, The American College of Obstetricians and Gynecologists (October 2012). "Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices". Obstetrics and Gynecology 120 (4): 983–88. doi:. PMID 22996129.
- ↑ Darney, Leon Speroff, Philip D. (2010). A clinical guide for contraception, 5th, Philadelphia: Lippincott Williams & Wilkins, 242–43. ISBN 978-1-60831-610-6။
- ↑ Black, K (October 2012). "A review of barriers and myths preventing the more widespread use of intrauterine contraception in nulliparous women". The European Journal of Contraception & Reproductive Health Care 17 (5): 340–50. doi:. PMID 22834648.
- ↑ ၄၂.၀ ၄၂.၁ ၄၂.၂ Gabbe, Steven (2012). Obstetrics: Normal and Problem Pregnancies. Elsevier Health Sciences, 527. ISBN 978-1-4557-3395-8။
- ↑ Steenland, MW (November 2011). "Intrauterine contraceptive insertion postabortion: a systematic review". Contraception 84 (5): 447–64. doi:. PMID 22018119.
- ↑ Roe, Andrea Hsu (2019-01-01). "Society of Family Planning clinical recommendations: contraception after surgical abortion" (in English). Contraception 99 (1): 2–9. doi:. ISSN 0010-7824. PMID 30195718.
- ↑ (2007) in Tommaso Falcone: Clinical reproductive medicine and surgery. Philadelphia: Mosby, 409. ISBN 978-0-323-03309-1။
- ↑ Grimes, D.A. (2007). ""Intrauterine Devices (IUDs)" In:Hatcher, RA; Nelson, TJ; Guest, F; Kowal, D". Contraceptive Technology.
- ↑ ၄၇.၀ ၄၇.၁ Marnach, ML (March 2013). "Current issues in contraception". Mayo Clinic Proceedings 88 (3): 295–99. doi:. PMID 23489454.
- ↑ Popularity Disparity: Attitudes About the IUD in Europe and the United States. Guttmacher Policy Review (2007). Archived from the original on March 7, 2010။ Retrieved on April 27, 2010။
- ↑ "The epidemiology of endometrial and ovarian cancer" (February 2012). Hematology/Oncology Clinics of North America 26 (1): 1–12. doi:. PMID 22244658.
- ↑ Hillard, Paula Adams (2008). The 5-minute obstetrics and gynecology consult. Hagerstwon, MD: Lippincott Williams & Wilkins, 265. ISBN 978-0-7817-6942-6။
- ↑ Deffieux, X (May 2011). "Tubal anastomosis after tubal sterilization: a review". Archives of Gynecology and Obstetrics 283 (5): 1149–58. doi:. PMID 21331539.
- ↑ ၅၂.၀ ၅၂.၁ ၅၂.၂ ၅၂.၃ Grimes, DA (Oct 18, 2004). "Fertility awareness-based methods for contraception.". Cochrane Database of Systematic Reviews (4): CD004860. doi:. PMID 15495128.
- ↑ Lawrence, Ruth (2010). Breastfeeding : a guide for the medical professional, 7th, Philadelphia: Saunders, 673. ISBN 978-1-4377-0788-5။
- ↑ ၅၄.၀ ၅၄.၁ Freundl, G (April 2010). "State-of-the-art of non-hormonal methods of contraception: IV. Natural family planning". The European Journal of Contraception & Reproductive Health Care 15 (2): 113–23. doi:. PMID 20141492.
- ↑ (November 1, 2011) "Fertility awareness-based methods", Contraceptive technology, 20th revised, New York: Ardent Media, 417–34. ISBN 978-1-59708-004-0. OCLC 781956734။
- ↑ "Mobile Phone Apps for the Prevention of Unintended Pregnancy: A Systematic Review and Content Analysis" (19 January 2016). JMIR mHealth and uHealth 4 (1): e6. doi:. PMID 26787311.
- ↑ ၅၇.၀ ၅၇.၁ Organization, World Health (2009). Medical eligibility criteria for contraceptive use, 4th, Geneva: Reproductive Health and Research, World Health Organization, 91–100. ISBN 978-92-4-156388-8။ Archived ဂျူလာင် ၉, ၂၀၁၂ at the Wayback Machine
- ↑ ၅၈.၀ ၅၈.၁ Jones, RK (June 2009). "Better than nothing or savvy risk-reduction practice? The importance of withdrawal". Contraception 79 (6): 407–10. doi:. PMID 19442773.
- ↑ Killick, SR (March 2011). "Sperm content of pre-ejaculatory fluid". Human Fertility (Cambridge, England) 14 (1): 48–52. doi:. PMID 21155689.
- ↑ ၆၀.၀ ၆၀.၁ Abstinence. Planned Parenthood (2009). Archived from the original on September 10, 2009။ Retrieved on September 9, 2009။
- ↑ (2007) Contraception Update, 2nd, New York: Springer, Abstract. doi:10.1007/978-0-387-32328-2_12. ISBN 978-0-387-32327-5။
- ↑ (Oct 5, 2009) Essential Concepts for Healthy Living. Jones & Bartlett Publishers, 116. ISBN 978-0-7637-5641-3။ 30 December 2017 တင်နိဿဲဏအ် ကလေင်စၟဳစၟတ်တုဲ။
- ↑ (2016) Exploring the Dimensions of Human Sexuality. Jones & Bartlett Publishers, 191. ISBN 978-1-4496-9801-0။ 30 December 2017 တင်နိဿဲဏအ် ကလေင်စၟဳစၟတ်တုဲ။
- ↑ "The limits of abstinence-only in preventing sexually transmitted infections" (2005). Journal of Adolescent Health 36 (4): 269–70. doi:. PMID 15780781.
- ↑ Kim Best (2005). "Nonconsensual Sex Undermines Sexual Health". Network 23 (4).
- ↑ (2017) The Oxford Handbook of Reproductive Ethics. Oxford University Press, 329. ISBN 978-0-19-998187-8။ 30 December 2017 တင်နိဿဲဏအ် ကလေင်စၟဳစၟတ်တုဲ။
- ↑ Thomas, R. Murray (2009). Sex and the American teenager seeing through the myths and confronting the issues. Lanham, MD: Rowman & Littlefield Education, 81. ISBN 978-1-60709-018-2။
- ↑ Edlin, Gordon (2012). Health & Wellness. Jones & Bartlett Learning, 213. ISBN 978-1-4496-3647-0။
- ↑ ၆၉.၀ ၆၉.၁ "Abstinence-Only-Until-Marriage: An Updated Review of U.S. Policies and Programs and Their Impact" (September 2017). The Journal of Adolescent Health 61 (3): 273–80. doi:. PMID 28842065.
- ↑ Kowal D (2007). "Abstinence and the Range of Sexual Expression", in Hatcher, Robert A.: Contraceptive Technology, 19th rev., New York: Ardent Media, 81–86. ISBN 978-0-9664902-0-6။
- ↑ Blackburn, Susan Tucker (2007). Maternal, fetal, & neonatal physiology : a clinical perspective, 3rd, St. Louis, MO: Saunders Elsevier, 157. ISBN 978-1-4160-2944-1။
- ↑ WHO 10 facts on breastfeeding. World Health Organization (April 2005). Archived from the original on June 23, 2013။
- ↑ "Lactational amenorrhea for family planning" (October 8, 2008). Cochrane Database of Systematic Reviews (4). doi:. PMID 14583931.
- ↑ ၇၄.၀ ၇၄.၁ ၇၄.၂ Fritz, Marc (2012). Clinical Gynecologic Endocrinology and Infertility, 1007–08. ISBN 978-1-4511-4847-3။
- ↑ Swisher, Judith Lauwers, Anna (2010-10-25). Counseling the nursing mother a lactation consultant's guide, 5th, Sudbury, MA: Jones & Bartlett Learning, 465–66. ISBN 978-1-4496-1948-0။
- ↑ What is the difference between emergency contraception, the 'morning after pill', and the 'day after pill'?. Princeton University (July 31, 2013). Archived from the original on September 23, 2013။ Retrieved on September 7, 2013။
- ↑ ၇၇.၀ ၇၇.၁ "Mechanisms of Action of Hormonal Emergency Contraceptives" (February 2010). Pharmacotherapy 30 (2): 158–68. doi:. PMID 20099990. “The evidence strongly supports disruption of ovulation as a mechanism of action. The data suggest that emergency contraceptives are unlikely to act by interfering with implantation”
- ↑ ၇၈.၀ ၇၈.၁ ၇၈.၂ ၇၈.၃ Shen, Jie (2019-01-20). "Interventions for emergency contraception" (in en). Cochrane Database of Systematic Reviews 1. doi:. PMID 30661244.
- ↑ Kripke C (September 2007). "Advance provision for emergency oral contraception". Am Fam Physician 76 (5). PMID 17894132.
- ↑ "Updates in hormonal emergency contraception" (September 2011). Pharmacotherapy 31 (9): 887–95. doi:. PMID 21923590.
- ↑ Richardson, AR (January 2012). "Ulipristal acetate: review of the efficacy and safety of a newly approved agent for emergency contraception". Clinical Therapeutics 34 (1): 24–36. doi:. PMID 22154199.
- ↑ Update on Emergency Contraception. Association of Reproductive Health Professionals (March 2011). Archived from the original on May 11, 2013။ Retrieved on May 20, 2013။
- ↑ "The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience" (2012). Human Reproduction 27 (7): 1994–2000. doi:. PMID 22570193.
- ↑ Glasier, A (Oct 2011). "Can we identify women at risk of pregnancy despite using emergency contraception? Data from randomized trials of ulipristal acetate and levonorgestrel". Contraception 84 (4): 363–67. doi:. PMID 21920190.
- ↑ "Dual protection against unwanted pregnancy and HIV / STDs" (1998). Sex Health Exch (3). PMID 12294688.
- ↑ ၈၆.၀ ၈၆.၁ "Dual Protection Against Unintended Pregnancy and Sexually Transmitted Infections: What Is the Best Contraceptive Approach?" (2002). Sexually Transmitted Diseases 29 (3): 168–74. doi:. PMID 11875378.
- ↑ Statement on Dual Protection against Unwanted Pregnancy and Sexually Transmitted Infections, including HIV. International Planned Parenthood Federation (May 2000). Archived from the original on April 10, 2016။
- ↑ Gupta, Ramesh C. (2011). Reproductive and Developmental Toxicology. Academic Press, 105. ISBN 978-0-12-382032-7။
- ↑ Bhakta, J (Nov 2015). "Teratogenic medications and concurrent contraceptive use in women of childbearing ability with epilepsy". Epilepsy Behav 52 (Pt A): 212–17. doi:. PMID 26460786.